Gut health may play an integral role in the prevention of HIV disease according to recent research. This may be surprising to learn as HIV is often considered in terms of sexual transmission and blood measurements of the virus, along with the CD4+T cells it infects and kills. But two thirds of the T-cells reside in the lymphoid tissue of the gut, meaning this is where the virus can easily be spread, even before it shows up within the blood.
Bloodwork has traditionally been the main focus for finding out about HIV because it’s easy to sample and broadly represents what is going on throughout the entire body. Access to the gut is more difficult, but researchers agree that better examination of it is required if more advances into the disease are to be continued.
Dysbiosis is a perturbation of the microbiome, allowing organisms within the gut to escape through the barrier wall and into the surrounding space before it enters the bloodstream. The dysbiosis is a general process involving various forms of disruption and different microbes, at locations roughly nine meters along the intestinal tract.
After conducting research into test subjects exposed to SIV – the simian equivalent of HIV, it was noted that there was “up to a 1,300 fold increase of bacteria circulating in the blood”. It was found that the number of bacteria increased in the blood before the SIV actually appeared in the blood and it was this that has led researchers to believe that the virus first attacks CD4+T cells that protect the gut wall from microbial translocation. But as the immune system begins to exercise control over the virus and the gut barrier function improves, the level of bacteria within the blood starts declining. Researchers from The Univeristy of Wisconsin-Madison believe that modulating this activity might reduce any initial burst of inflammation that can fuel the HIV infection and establish viral set points and the seeding of reservoirs.
On the Pacific Coast, researchers administered a probiotic to the infected test subjects to modulate a more favourable microbial system within the gut and to improve immune function. The results found an increase in IgG (immunoglobin) producing B cells in both the colon and lymph nodes. This finding suggests that by enhancing the immune response in the gut, it could work as a means to increase immune responses to vaccination that are otherwise typically weaker in those affected with HIV, the elderly or other persons at risk.
Meanwhile, researchers from The Harvard Medical School and the Ragon Institute found that HIV affects the human gut microbiome and that there is very little difference between the samples of the 145 gut-positive people in Boston and the HIV-positive in Uganda, with the most significant difference being seen in the Boston set. The healthy HIV-negative Bostonians were the outliers, and the guts of the other three groups were similar, especially for the untreated persons on both continents. The HIV-uninfected patients were shown to have much greater richness in their samples, along with a unique population that was primarily composed of the bacteria from the phylum Fermicutes.
A gastroenterologist from The University of California researched into FMT (Fecal Microbial Transplantation) and found that the subjects experienced the same few side effects as the patients who tried FMT. The main problem however is that the transplanted organisms failed to survive and supplant the bugs that were already present and causing the dysbiosis. The researchers weren’t surprised however as it’s been recognised that C.difficile and a combination of antibiotics can wipe out the bacteria in the gut, so transplanted organisms have little competiton in colonizing the gut.
Probiotics Can Support Gut Health
Taking a good probiotic is recommended if you want to support your gut health and improve your immune system. When the gut has healthy microflora it is better able to fight off any bad bacteria that may invade the body. For this reason, a probiotic can help to promote the growth of various Lactobacillus bacteria as these have the most beneficial effects within the gut. One probiotic that is suggested is Prescript-Biotics from Good Health Naturally, due to it being a combination of 29 probiotic microflora combined with a humic/fulvic acid prebiotic to enhance SBO proliferation. Prescript-Biotics contains a colony forming unit of 145 million per capsule, which isn’t comparable to CFU’s in lacto and bifido based probitoic products where the large numbers (billions) are used to rectify the massive loss (99%) that occurs during the manufacturing, storage and the stomach acid degradation process. This is why Prescript-Biotics is in a different league compared to most ordinary probiotic supplements when it comes to providing protection for your gut health and building up your immune system against potential infections.
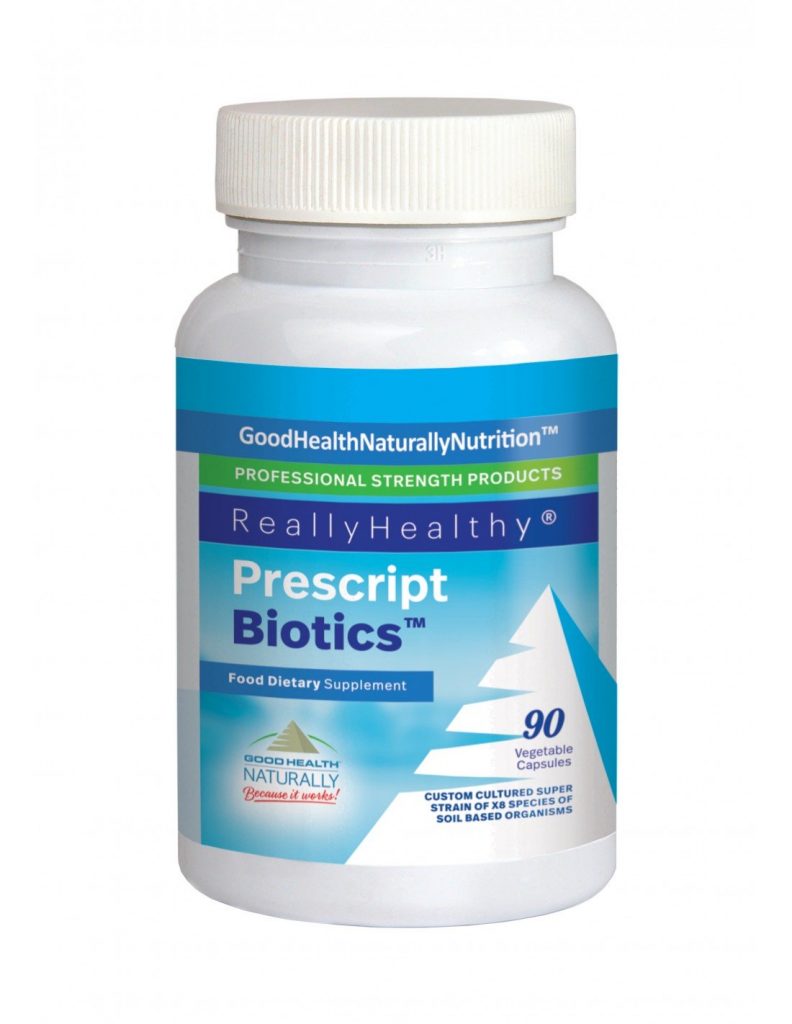 Prescript-Biotics™ – Recommended to support a healthy and strong immune system. SBOs in PrescriptBiotics™ are cultured together and encapsulated with their own ancestral food source to keep them vital and living: a humic and fulvic acid prebiotic made from minerals that are billions of years old and extracted from deep inside the earth.
Prescript-Biotics™ – Recommended to support a healthy and strong immune system. SBOs in PrescriptBiotics™ are cultured together and encapsulated with their own ancestral food source to keep them vital and living: a humic and fulvic acid prebiotic made from minerals that are billions of years old and extracted from deep inside the earth.
PrescriptBiotics™ capsules are pure, chemical-free, toxin-free, GMO-free, nutrient-rich, and naturally dehydrated to avoid damage done in the freeze-drying process.
Recommended Dose: Take 1 capsule a day. Increase by one capsule a day, for each week.
Available from Good Health Naturally.




